Implementing a prenatal care tool in routine OB care
In collaboration with Advocate Aurora Research Institute, funded by the Robert Wood Johnson Foundation (2020).
Kim Erwin
Director, Equitable Healthcare Lab; Associate Professor of Healthcare Design and Design Methods
Veronica Fitzpatrick
Research Scientist, Advocate Aurora Research Institute
Anne Rivelli
Epidemiologist, Advocate Aurora Health
Maureen Shields
Epidemiologist, Advocate Aurora Health
CHALLENGE
How to design uptake of a prenatal care tool in routine care?
Testing new interventions in real-world clinical settings is essential to building evidence. But provider uptake of short-term pilot interventions is a known challenge for researchers.
APPROACH
The CONTINUE study blended methods from Human-Centered Design and Implementation Science to design an implementation strategy to promote and assess uptake of a pregnancy support tool in three clinics. We engaged 71 patients and 20 OBs, residents, nurses and midwives across clinics in a multi-phased approach:
Phase 1 tailored the tool and implementation plan to the clinics and patient population;
Phase 2 developed clinic-specific implementation supports;
Phase 3 conducted a series of 14-week pilot tests (4 total) with 4 provider types;
Phase 4 used interviews and surveys to assess provider and patient experiences. We used the Implementation Outcomes framework (Proctor et al) to evaluate the intervention’s acceptability, appropriateness, feasibility, fidelity and sustainability. A card sorting activity also assessed the tool’s performance against stakeholder-identified benefits.
OUTCOME
The CONTINUE pilot showed high and rapid rates of adoption by both patient and provider implementation measures. Of the implementation outcomes, feasibility received the highest overall score, indicating all provider types felt the tool was practical to use in their current practice. All scores varied by provider type, with OB Attendings and Midwives consistently scoring highest in all implementation measure categories, especially fidelity. This suggests they are the appropriate provider for full implementation.
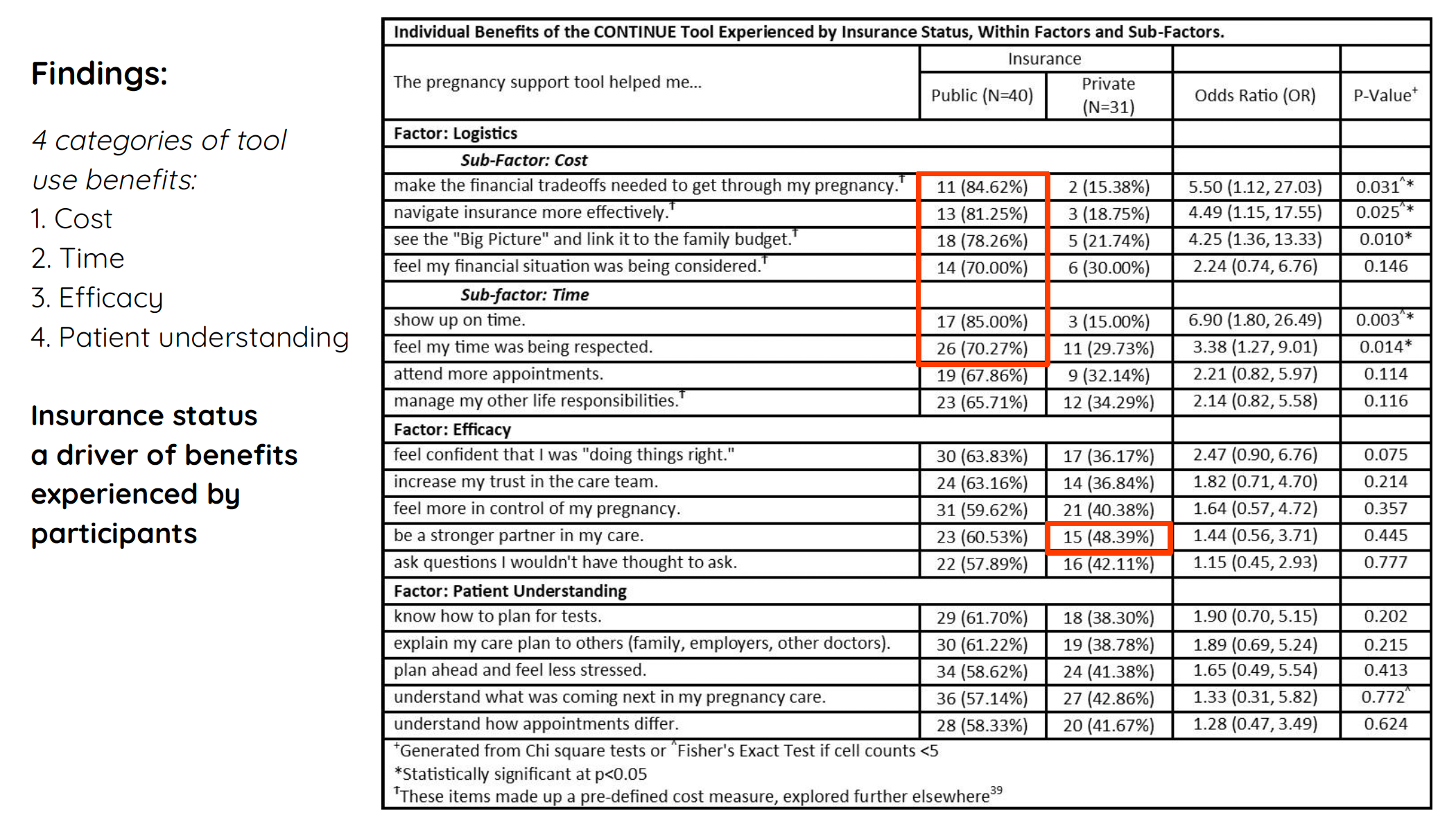
Lower-income patients benefitted most: insurance status — a proxy for income — was highly correlated with reported benefits. The 18 patient-reported benefits were clustered using Exploratory Factor Analysis. This produced 4 benefit clusters: cost, time, self-efficacy, and understanding. While 92% of participants reported experiencing at least 1 of 4 benefit clusters, those with public insurance had 4-5 times greater odds of experiencing cost and time benefits when using the tool.
ADDITIONAL FILES
Journal of Primary Care and Community Health
American Journal of Applied Mathematics and Statistics